29 Nov Improving Brain Health by Reducing Inflammation
There are many recent studies looking at the possible link between inflammation and psychiatric illness. If neuroinflammation plays some role in causing psychiatric disorders, then there is reason to believe that reducing neuroinflammation may be considered as a useful line of treatment and even a way to improve brain health.
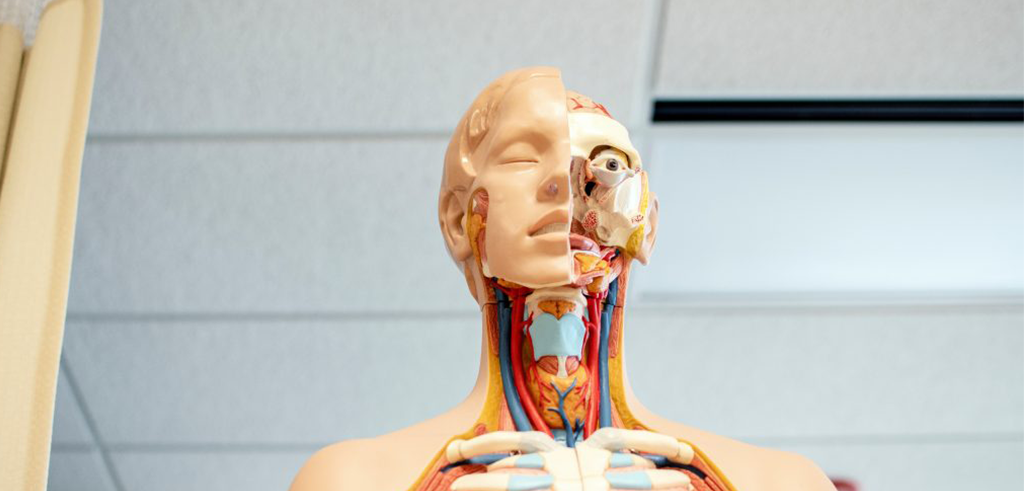
Brain Health is Mind Health
A 2013 review article by Najjar et al. looked at evidence reviewing the role of neuroinflammation in several psychiatric disorders.
The article argued that, ‘as biological abnormalities are increasingly identified among patients with psychiatric disorders, the distinction between neurological and psychiatric illness fades.’
As physical injuries and abnormalities including head trauma, the damage caused by stroke, and brain tumours have been shown to impact psychiatric symptoms, it becomes increasingly difficult to hold a view of brain health and mind health as separate.
Today, the study of the possible link between neuroinflammatory and immunological abnormalities and patients with classical psychiatric disorders further reinforces that the body (or the physical brain) and the mind are not separate, and that illness or abnormalities of the physical brain can play a role in mental health.
The Najjar et al. article also looked at studies discussing the role of the blood-brain barrier (BBB) in some conditions. This is an area of growing research interest, particularly in the development of Alzheimer’s disease and epilepsy.
In the brain, mediators that occur when inflammation is present are known to also impair neurotransmission. Primed microglia are one of the primary causes of brain inflammation. All over your brain and nervous system are cells called microglia. Their role is to protect your neurons and nerve cells. These cells can become activated by an initial insult. This is known as priming. Examples of an initial insult that can turn your microglia into primed microglia include head injuries, concussions, infections, Covid-19, and high emotional/psychological stress.
Your microglia have a threshold for being activated into attack mode. This activated mode sets the cycle for brain inflammation. It may not happen to all parts of your nervous system. It will happen to the areas that have primed microglia. After the initial insult that primed them, they will always be on guard and immediately react to triggers, causing brain inflammation symptoms.
This is one reason why the brain is usually protected by the BBB – to only allow vital nutrients and amino acids like L-Tryptophan into the brain where, for example, the L-Tryptophan is converted into serotonin, yet at the same time stopping any toxins from entering. Excitotoxins, should they enter, will lead to a cascading inflammatory response as a way to try and protect the brain, but may end up doing damage to the neurons themselves.
Strokes, epilepsy, or other diseases can compromise the BBB and lead to its breakdown. It is also now emerging that when the first protective barrier, the ‘gut barrier’ is compromised, that this paves the way for more toxins to enter the blood and move to directly attack the BBB. Just like this leaky gut barrier, eventually, the BBB becomes leaky too. This process is increasingly being adopted to explain the increased prevalence of psychiatric conditions in these circumstances. Having a ‘leaky’ BBB can have serious implications for inflammation and for brain health.
Lee and Giuliani in their more recent 2019 research article, described the link between depression, fatigue, and increased immune activation, the psychological effect of pro-inflammatory insults, and the treatment efficacy of anti-inflammatory medications, providing convincing evidence supporting the hypothesis that inflammation plays a role in the causation of some forms of depression and fatigue.
A review of emerging research and clinician opinion on the more commonly occurring conditions like attention-deficit/hyperactivity disorder (ADHD), autism, depression and Alzheimer’s disease will quickly lead you to the conclusion that they are multisystemic in their cause yet ultimately linked with inflammatory processes within the body and brain.
According to a 2018 study published in Biological Psychiatry by Sonja Stojanovski et al., physical brain injury in children contributes to the development of ADHD, distinct from the more well known genetic form of the disorder. Mild traumatic brain injuries like concussions are quite common in children and adolescents they concluded, and should be screened for when assessing and diagnosing ADHD. It is interesting to note, that many of the issues within the brains of those suffering post-concussion syndrome stem from the inflammatory response that occurs within the brain and this lends more argument for better ways to identify and address inflammatory responses. This paper strongly argues, and I support this argument, for a more personalised medicine approach that seeks to look more closely at the brain and other causal factors. This is one reason why at Neuroperformance we use quantitative electroencephalography (QEEG) ‘brain scans’ to look more closely.
Treating Inflammation and the Outcomes for Brain Health
Both the 2013 Najjar et al. review article and a 2017 review article by Radtke et al. took the assumption that if inflammation can play a role in the development and progression of psychiatric disorders, then anti-inflammatory treatments may play a role in the treatment of these disorders.
Both articles considered studies where anti-inflammatory treatments were trialled. These included common non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin and ibuprofen, as well as omega-3 fatty acids, amongst others.
The Najjar et al. article sought to understand how the outcomes of these studies could point to the most promising treatments for use in both a preventative capacity and for the relief of symptoms.
The Radtke et al. article concluded that although these anti-inflammatory treatments had not translated into clinical treatment at the time of writing, that adjunctive therapy with anti-inflammatory medication proved promising as a novel route to treatment of psychiatric diseases. This could especially be the case where conventional therapy has failed in the treatment of these conditions.
There are small, yet compelling studies showing the benefits of omega-3 supplements for treating depression, for example, and it is believed that its benefit is derived through the anti-inflammatory process. Vitamin D has also been shown to improve depression, and although it is vital for the production of many chemicals within our body and brain, it is also anti-inflammatory. These more ‘natural’ compounds carry powerful properties that are now understood by science and well documented and should not be dismissed simply because they are ‘natural’.
How to Address Neuroinflammation and Improve Brain Health
I have come to the conclusion that neuroinflammation is caused by multisystemic issues, and so it stands to reason that any approach that seeks to address this driver of poor brain and mental health MUST seek to address several areas at once to reap the benefits.
It is also wise counsel to acknowledge that there is no quick fix, and often treatment will take many months to be effective and many more months to see real, sustainable change.
The key areas within my N.E.U.R.O program that should all be worked on within a complex systems mindset include Nutritional supplementation & food, Exercise (or more so specifically daily movement), Unwinding (stress management/disconnecting daily from technology) Restorative sleep (our most efficient brain detox process) and Optimising brain plasticity with targeted brain strengthening exercises like neurofeedback, neurogames, reading, dancing, or learning a new language.
Many of my patients are seeking some immediate help and need immediate support for motivation, mood, and attention that leads to targeted supplements often being the first line support to help underpin being able to implement all the other vital lifestyle changes. I will always recommend a good quality, high potency omega-3 and vitamin D supplement. Omega-3’s are truly one of the best ways to address inflammation. Curcumin is also proving to be very effective and has been shown to improve brain function. One of my favourites is N-acetyl cysteine, a potent amino acid able to cross the BBB and directly impact inflammation in the brain along with neurotransmitter and cellular repair benefits.
An exciting development with building research support is the use of photobiomodulation helmets for the treatment of Alzheimer’s dementia and Parkinsons, showing real promise in addressing brain inflammation, restoring neuronal damage, and thus improving the symptoms of poor memory and mood. It is one of many reasons why I have added into my clinic the use of photobiomodulation as a treatment as one more tool to try and support brain recovery within traumatic brain injury (TBI), dementia, or other neuroinflammatory linked conditions.
If you love your brain and want to remain on your game, why not seek an individual assessment to determine your personalised treatment pathway to better brain health, mood, and performance.
Articles cited:
Souhel Najjar, Daniel M. Pearlman, Kenneth Alper, Amanda Najjar, Orrin Devinsky, “Neuroinflammation and psychiatric illness.” Journal of Neuroinflammation 2013 10:43.
Franziska A. Radtke, Gareth Chapman, Jeremy Hall, Yasir A. Syed, “Modulating Neuroinflammation to Treat Neuropsychiatric Disorders”, BioMed Research International, vol. 2017.
Chieh-Hsin Lee, Fabrizio Giuliani, “The role of Inflammation in Depression and Fatigue” Front Immunol. 2019; 10: 1696. Published online 2019 Jul 19. doi: 10.3389/fimmu.2019.01696
Sonja Stojanovski et al. Polygenic Risk and Neural Substrates of Attention-Deficit/Hyperactivity Disorder Symptoms in Youths With a History of Mild Traumatic Brain Injury, Biological Psychiatry (2018). DOI: 10.1016/j.biopsych.2018.06.024
This post may contain links for affiliate products for which I receive a commission at no cost to you.



